156,242 Too Many: A Look at Our Nation’s Pain, Plus an Antidote for it
Standout deaths of despair statistics and solutions from a newly released Well Being Trust & Trust for America’s Health report
Earlier this week, Well Being Trust and Trust for America’s Health released their annual report Pain in the Nation – a comprehensive look at how many American lives we’ve lost to alcohol, drugs and suicide, aka deaths of despair, from year to year.
This year’s report is especially important. While the data is from 2019 – the latest available from the CDC’s Multiple Cause of Death database – it presents that information alongside statistics signaling how America’s mental health has worsened during this pandemic, and therefore how severe the nation’s pain may be next year and the year following if we don’t put solutions in place immediately.
What kind of data are we talking (or reading, rather)? And as a country, what does that call on us to do?
Well, let’s get into it.
THE DATA
All things considered, in 2019, 156,242 Americans died due to alcohol, drugs or suicide. 39,043 of those deaths were tied to alcohol misuse – a 4%increase over 2018 – and drug-induced deaths in 2019 increased by 5% to account for 74,511 of that total.
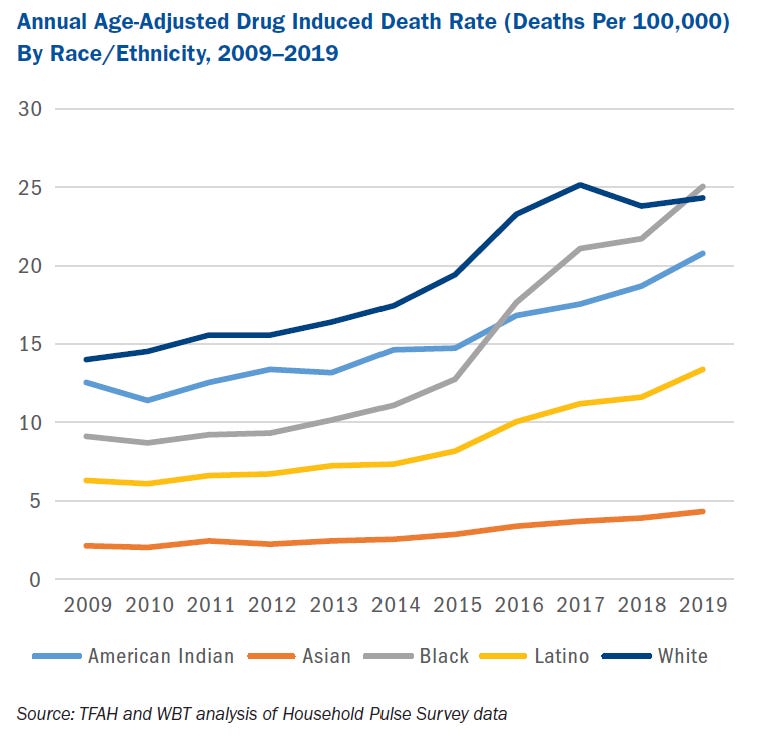
There are multiple standout statistics within this category of drug-induced deaths. One of the most notable is the fact that while overall drug-induced deaths increased, deaths due to natural/semisynthetic/prescription opioids and heroin decreased. Another is the fact that, for the first time since 2005, the 2019 drug deaths rate for Black people was higher than that of whites. Drug-induced deaths were up by 15 percent among Latinos and Blacks, 11 percent for American Indians and 10 percent for people of Asian descent, a stark contrast to the 2 percent increase in drug-induced deaths among whites.
Demographic-specific statistics on alcohol-related deaths are also interesting, the highest being among American Indians (31.9 deaths per 100,000 people), adults over 55 (28.3 deaths per 100,000 people) and males (15.2 deaths per 100,000 people) – recall my recent post on addressing the latter population. However, another standout statistic is this: The suicide rate went down by 2% in 2019. The age-adjusted suicide rate declined from 14.2 to 13.9 deaths per 100,000 deaths, bringing the 2019 total to 47,511.
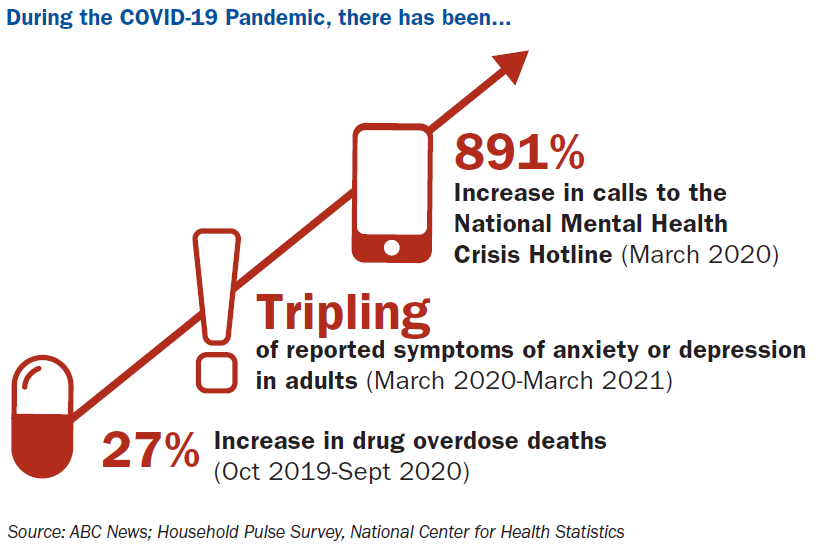
This may or may not come as a shock to you. Suicide was oft a hotly contested topic of conversation during this pandemic, with horrifying stories about teen suicide, particularly in Las Vegas, fueling calls to schools to reopen. The concern was certainly justified this past school year, data from the CDC finding that compared with 2019, the proportion of mental health–related visits to Emergency Departments for children aged 5–11 and 12–17 years-old in 2020 increased approximately 24% and 31%, respectively. But that concern should probably hold through this school year too, because poor mental health is never caused by one singular thing, and the extent to which one year of social isolation and uncertainty impacted us isn’t something that’s going to vanish overnight. Case in point, calls to the Substance Abuse and Mental Health Services Administration Disaster Distress Helpline increased by 891 percent between March 2019 and March 2020, a June 2020 CDC study found that 13 percent of adults “started or increased substance use to cope with pandemic-related stress or emotions,” and the number of adults reporting symptoms of anxiety or depression from March 2020 through March 2021 was triple the number who reported such symptoms in 2019.
THE TRENDS
I know those are a lot of numbers to throw at you all at once. So. let’s take a look at the trends to extract some of the greatest takeaways here.
Since the greatest takeaway ties nicely to what comes next, I’m not going to invert the pyramid this time around. I’m going to call out takeaways for each cause of death separately, before calling out the bigger-picture problems.
Where alcohol-related deaths are concerned, 2019 was the tenth year in a row that these deaths increased. Americans are increasingly turning to alcohol to cope with the everyday stressors – money, child care, health care, and other things that the American Families Plan sought out to address – and it’s literally killing them.
Where drug-induced deaths are concerned, deaths are still increasing, but there are distinct changes among whom, and from what, that we should keep an eye on in the months to come. Like I already mentioned, the rate at which Black Americans are dying from drug use is outpacing the rate at which white Americans are dying from drug use – the historic trend of drug overdoses among whites substantially outpacing other racial groups may be changing. Similarly, while prescription opioids were driving drug deaths higher over the last few years, now, synthetic opioids – think fentanyl, cocaine and other psychostimulants like methamphetamine and ecstasy – are driving drug-induced deaths higher (up 16%, 8% and 28%, respectively) and opioid prescriptions less so.
Where suicide deaths are concerned, we can breathe a very small sigh of relief. While the 2019 decline in suicide deaths is statistically significant and noteworthy considering it's the first decline since 2005, we should see this as a bright spot, but not get comfortable quite yet. No single data point determines a trend, and clearly our work is still cut out for us …
… which brings me to the most important thing you – and everyone you know! – needs to understand about this year’s Pain in the Nation report: Overall, deaths due to alcohol, drugs and suicide are still steadily increasing, despite the fact that we’ve known about these increases for ten years now! In the last decade (2009 – 2019) the number of American who’ve died from these deaths of despair have increased by a whopping 52%. Why? Because we have yet to have a much-needed national response. Enter my recent series on the need for a National Mental Health Rescue Plan, and the even more tailored solutions shared below.
THE SOLUTIONS
156,242 lives lost each year is 156,242 too many. We need to see America’s mental health crisis as the public health crisis that it really, truly is – a crisis that has consistently killed roughly one-fifth that of Covid-19 – and more importantly, we need to immediately respond by investing in prevention and conditions that promote health, addressing the worsening drug use and overdose crisis, and transforming the mental health and substance use prevention system.
To accomplish each, here’s where leaders should focus their efforts:
Invest in Prevention and Conditions that Promote Health
· Reduce traumatic experiences, and promote resilience in children, families, and communities.
· Expand substance use prevention, mental health, and resiliency programs and staff in schools.
· Bolster crisis-intervention programs and supports.
· Reduce availability of illicit opioids and inappropriate prescriptions.
· Lower excessive alcohol use through evidence-based policies.
· Limit access to lethal means of suicide, including drugs and firearms.
Address the Worsening Drug Use and Overdose Crisis
· Implement policies targeting psychostimulant use.
· Promote harm-reduction policies to reduce overdose and blood-borne infections.
· Continue pandemic-related enhanced flexibilities in access to and rules for substance-use treatment.
· Address the secondary impact of the substance use and overdoses on children.
Transform the Mental Health and Substance Use Prevention System
· Expand efforts to combat stigma and improve social attitudes toward mental health.
· Improve data accuracy, completeness, and timeliness through innovation and additional funding.
· Modernize mental health and substance use services.
· Increase access to mental health and substance use healthcare through full enforcement of the Mental Health Parity and Addiction Equity Act.
· Expand the mental health and substance use treatment workforce.
· Build community capacity for early identification and intervention for individuals with mental health needs.
· Promote diversity and culturally appropriate care in the healthcare system.
· Adopt trauma-informed and culturally competent policies and practices for youth-serving programs and agencies.
But if you aren’t in politics, don’t count yourself out, reader. As I end the majority of my posts, I want to remind you that solving America’s mental health and addiction crisis is a shared responsibility. Policymakers have a huge part to play in making sure you have easy access to the training and care you and your loved ones need, but you do too. (And you may even be able to help push them to make the changes you want to see once you’ve read through this series.)
Because when I look at the number of deaths in this report – the trends – I tire of saying year after year “the most ever seen.” Our trends are disturbing and it is on us to do something about it. This is not a moment for timidity, but of courage – to stand up for a new way of thinking about mental health and addiction. To stop chasing money for the moment, and to develop an actual strategy for our structure, because it’s hard to see how more money into the current system and structures does anything to change our outcomes. Let’s not pretend it does.
Mental health is all our responsibility, and this is our moment to pursue something radical – something that demonstrates an understanding of the fact that the solutions to our problems are not more of the same.
The nation is in pain. It’s on all of us, everywhere to help heal it.